Mobile:Best viewed horizontally
![]()
Let’s start with the basics! What exactly IS osteoarthritis?
Osteoarthritis, or OA, is a condition that affects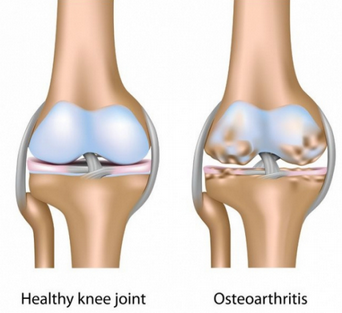 the cartilage of our joints and is a normal part of getting older. Protective cartilage covers the ends of our bones to assist with shock absorption, such as when we run or jump, and keeps movements at our joints smooth by limiting friction between the bones. As we age, the cartilage in our bodies begins to gradually deteriorate and can change the structure and function of the joint – this degeneration is known as OA.
the cartilage of our joints and is a normal part of getting older. Protective cartilage covers the ends of our bones to assist with shock absorption, such as when we run or jump, and keeps movements at our joints smooth by limiting friction between the bones. As we age, the cartilage in our bodies begins to gradually deteriorate and can change the structure and function of the joint – this degeneration is known as OA.
 Now that we understand OA, What are the symptoms?
Now that we understand OA, What are the symptoms?
The first thing that most people notice is pain, usually occurring during or after activity. You might have knee pain following a run or long walk, while going up and down stairs, or with repetitive movements like squats or lunges. In other cases, joint stiffness is the most prominent symptom. You may find that first thing in the morning or after sitting for longer periods of time the knee doesn’t move as easily.
As osteoarthritis progresses it is common to see less movement and find that the knee doesn’t bend or straighten as far as it once could. Many people also experience a grinding feeling and hear popping or clicking noises. It is important to note however, that popping and clicking doesn’t always indicate OA. It is also normal to notice periodic swelling due to the inflammation of the muscles, tendons, and ligaments around the joint.
Are some people more susceptible to OA than others?
As a degenerative joint condition older adults are more likely to have osteoarthritis in their joints than the younger population. Remember that age-related joint changes are NORMAL and do not always correlate with the symptoms of OA. Studies show that osteoarthritis is more common in women than in men after the age of 55. It is thought that the varying hormones between men and women are responsible for this difference. Extra weight and obesity mean more pressure on the knees when we walk, run, or stand up, and can contribute to the breakdown of cartilage leading to OA. Therefore maintaining a healthy weight with proper diet and exercise can help to reduce your risk of osteoarthritis. Multiple injuries to the same joint, such as torn cartilage or ligament sprains, and repetitive stress from a job or sport can also increase your likelihood of having OA. Our genetics do play a role in the health of our joints and a family history of osteoarthritis could mean that you are more susceptible.
 Many, if not ALL, symptoms of osteoarthritis can be controlled.
Many, if not ALL, symptoms of osteoarthritis can be controlled.
Although the physical changes of the joint associated with OA (often identified on x-rays) cannot be reversed, exercise, maintaining a healthy weight, self-management strategies, and physiotherapy intervention can lead to a decrease in pain as well as an increase in movement, strength, and function for those with osteoarthritis. It is essential to understand that what is shown on an x-ray does not always accurately represent one’s symptoms. For example, when an x-ray finds degenerative changes in the knee joint it does not guarantee that the person will have pain, stiffness, or loss of movement. It is possible to have minimal to no pain and show severe changes upon x-ray or to have severe pain with minimal degenerative changes – every knee is unique!
How can physiotherapy treat OA?
 Your physiotherapist can design a specific exercise program to help you meet your goals – whatever they may be. Did you know that regular exercise can decrease pain, regain and maintain movement, improve endurance, and increase strength to limit the symptoms of osteoarthritis? Now you do! In order to properly manage your OA it is important to listen to your body and incorporate self-management strategies so you can continue to function pain free. Ask your physiotherapist how you can help to limit the symptoms of osteoarthritis at home! How can physiotherapy treat OA?
Your physiotherapist can design a specific exercise program to help you meet your goals – whatever they may be. Did you know that regular exercise can decrease pain, regain and maintain movement, improve endurance, and increase strength to limit the symptoms of osteoarthritis? Now you do! In order to properly manage your OA it is important to listen to your body and incorporate self-management strategies so you can continue to function pain free. Ask your physiotherapist how you can help to limit the symptoms of osteoarthritis at home! How can physiotherapy treat OA?
For people with advanced joint degeneration in their knees, wearing a brace during activity or using a cane for longer distances may be the best option. Be sure that these devices fit you properly before starting to use them! physiotherapists will often use hands-on treatment such as joint movements and massage as well as modalities like hot or cold packs, acupuncture, and ultrasound or TENS machines to improve movement and decrease pain.
Regular exercise can limit the symptoms of osteoarthritis.
 One of the best things you can do to limit the impact that osteoarthritis has on your day-to-day life is to remain active! It is recommended that we get 150 minutes of physical activity each week. If you’re new to exercising try 10 to 15 minutes at a time and work your way up! In order to successfully commit to daily exercise it is important to do something you enjoy.
One of the best things you can do to limit the impact that osteoarthritis has on your day-to-day life is to remain active! It is recommended that we get 150 minutes of physical activity each week. If you’re new to exercising try 10 to 15 minutes at a time and work your way up! In order to successfully commit to daily exercise it is important to do something you enjoy.
Cycling, yoga, swimming, group fitness, aquasize, and tai chi are all great options!
Providing weight-bearing activities, like walking, doesn’t increase your pain, it is suggested that you continue with these activities to maintain healthy bones.
Types of exercise that are sometimes left behind are stretching and strengthening. Incorporating both of these will build muscle to support knees with OA and maintain or improve the flexibility of our joints. As we previously mentioned, we have to listen to our bodies and sometimes it’s challenging to know what we should be feeling. If you have osteoarthritis, you should be avoiding activities that cause an increase in pain, however it is normal to have a pulling sensation with stretches or muscle soreness following a workout.
Always confirm with your physiotherapist that an exercise is right for you before beginning something new!
Understanding how to properly use heat and ice is important.
 One of the number one questions that we are asked as physiotherapists is “which is better – heat or ice?”. The short answer is it depends! Heat will help to loosen up muscles and joints to improve movement and flexibility, while ice is great to reduce pain and swelling. Always keep a protective layer of clothing or a towel between your body and the hot or ice pack to avoid a burn or skin irritation!
One of the number one questions that we are asked as physiotherapists is “which is better – heat or ice?”. The short answer is it depends! Heat will help to loosen up muscles and joints to improve movement and flexibility, while ice is great to reduce pain and swelling. Always keep a protective layer of clothing or a towel between your body and the hot or ice pack to avoid a burn or skin irritation!
Learn how you can help relieve the stress on your knee joint.
 Physiotherapists often incorporate hands-on techniques into our treatment to reduce your joint pain. One of the methods we use is something called traction. This means that we are creating a little more space between the bones of the knee joint that may be reduced due to the cartilage degeneration seen in OA.
Physiotherapists often incorporate hands-on techniques into our treatment to reduce your joint pain. One of the methods we use is something called traction. This means that we are creating a little more space between the bones of the knee joint that may be reduced due to the cartilage degeneration seen in OA.
We encourage you to replicate this at home by sitting on a stool or tall chair with your feet lifted off the floor while wearing a shoe or ankle weight. You are welcome to add small swinging or circular movements to increase the gentle pull through the knee joint.
Will I need a cane or brace?
 As osteoarthritis progresses many people will prefer the help of a brace, cane, walker, or grab bars, to continue enjoying an active lifestyle or maintain independence. These devices can decrease pain by relieving pressure, increase joint stability by providing support, reduce your risk of falls, and are an important part of managing OA! Speak to your doctor or physiotherapist to determine if one of these is the best option for you.
As osteoarthritis progresses many people will prefer the help of a brace, cane, walker, or grab bars, to continue enjoying an active lifestyle or maintain independence. These devices can decrease pain by relieving pressure, increase joint stability by providing support, reduce your risk of falls, and are an important part of managing OA! Speak to your doctor or physiotherapist to determine if one of these is the best option for you.
